Addictive substances and behaviours
We can become addicted both to substances and to behaviours.
Substances
Addiction to substances can take the form of excessive use of, and dependence on:
- Alcohol
- Tobacco
- Certain prescription medications
- Illicit drugs such as ecstasy, cocaine, or heroin
Behaviours
Addiction to behaviours can take the form of being excessively dependent on performing an activity or having an experience. For instance, we can become addicted to:
- Sex
- Gambling
- Exercise
- Pornography
- Over-eating
- Under-eating
Around half of all people with addiction engage in more than one type of addictive behaviour.
George Ainslie, the psychiatrist and behavioural economist, summarises the matter by writing that:
Addictive behaviour occurs when people repeatedly choose pleasure now without worrying about future pain.Szalavitz, M. (2016). Unbroken Brain. New York, NY: Picador, p.161.
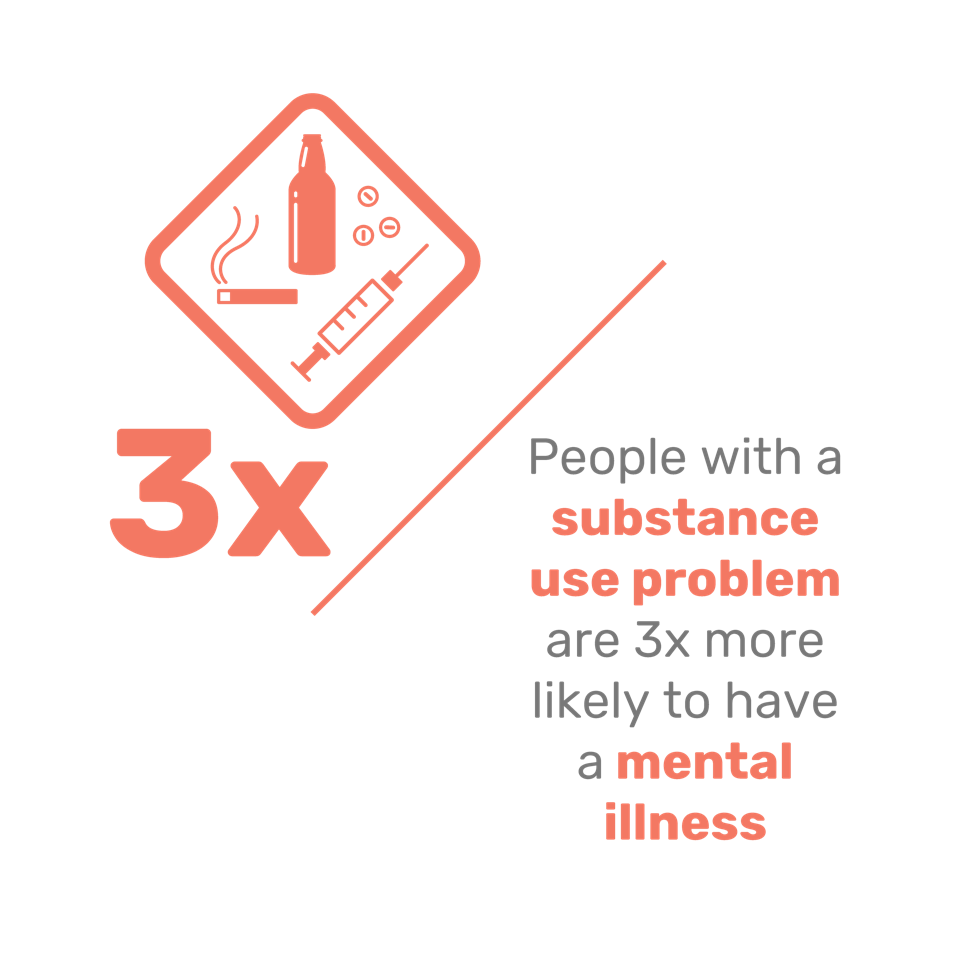
Addiction and mental health
Rush et al. (2008). Prevalence of co-occurring substance use and other mental disorders in the Canadian Population. Canadian Journal of Psychiatry, 53, pp. 800-9.
Addiction can be both a symptom of mental health issues, and a contributor to them.
There is a very strong correlation between mental health issues and addiction.Bussing-Birks, M. (2017). ‘Mental illnsss and substance abuse’. National Bureau of Economic Research. [online] Available at: http://www.nber.org/digest/apr02/w8699.html [acccessed 2 Nov. 2017]. At least 50% of people with addiction – according to some studies, as high as 98% – have a mental health condition.
Addiction can both trigger and be triggered by:
- Depression
- Anxiety
- Insomnia
- Obsessive Compulsive Disorder (OCD)
- Attention Deficit Hyperactivity Disorder (ADHD)
- Psychosis
- Bipolar disorder
Addiction as a contributor to mental health issues
Being addicted to substances or behaviours can negatively impact our mental health. It can also cause physical problems, which may in turn contribute to mental health issues.
The habitual use of toxic and addictive substances can cause:
During intoxication, or the acute stages of withdrawal, addicted people may experience:
- Mood swings
- Impaired judgement
- Cognitive impairment
- Insomnia
- Severe anxiety
- Psychosis
Chronic addiction can also alter the body’s biochemistry, and directly or indirectly contribute to nutritional and physiological imbalances such as hormone and neurotransmitter imbalances.Lake, J. (2009). Integrative Mental Health Care. New York, NY: W.W. Norton & Co., p.260.
These in turn can contribute to, or exacerbate, mental health issues:
The long-term abuse of drugs and alcohol can contribute to structural and chemical changes in the brain. This can affect many of its functions, including our judgement, decision-making, stress levels, memory, and behaviour.National Institute on Drug Abuse. (2014). ‘Drugs and the brain’. [online] Available at: https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain [accessed 2 Nov. 2017].
Addiction can change our brain chemistry, in particular our neurotransmitter balance. For instance, heavy substance use can cause the repeated release of dopamine (a neurotransmitter controlling the brain’s pleasure centres). Over time, the brain may respond by reducing its production of dopamine, or its number of dopamine receptors.Scott, T. (2011). The Anti-Anxiety Solution. Oakland, CA: New Harbinger Publications, p. 64.
We then need more of the substance to keep feeling the same levels of pleasure. This can make it harder for us to give it up, leading us to consume it in greater amounts. This in turn, can worsen the other effects of addiction.
Chronic alcoholism and drug addiction can contribute to a range of nutritional deficiencies and blood sugar issues. These in turn can contribute to, or exacerbate our mental health symptoms, and increase our desire to self-medicate further.
Some examples of these problems include:
Mineral and electrolyte imbalances
Mineral and electrolyte imbalances are extremely common among addicted individuals, due to a poor diet and regular diarrhoea. This can lead to the depletion of natural stores of copper, iron, magnesium, and zinc. It may also cause deficiencies in sodium, calcium, or potassium, which can, in extreme circumstances, prove fatal.Nabipour, S., Ayu Said, M., Hussain Habil, M. (2014). ‘Burden and nutritional deficiencies in opiate addiction – systematic review article’. Iranian Journal of Public Health, 43(8), pp.1022–1032.
Vitamin imbalances
Many alcoholics have abnormally low blood levels of vitamins A, B (especially thiamine, folate, and B6), and C, all of which are essential to mental health. In particular, a lack of vitamin B6 can cause mental confusion and skin problems, while a lack of B1 can cause alcoholic dementia and cardiovascular issues.Lake, J. (2009). Integrative Mental Health Care. New York, NY: W.W. Norton & Co., pp. 260–265.
Essential fatty acid imbalances
Addicted people often show marked deficiencies in certain essential fatty acids, which are central to the brain’s production of hormones and other brain chemicals, and therefore to our mental health.Lake, J. (2009). Integrative Mental Health Care. New York, NY: W.W. Norton & Co., p. 261.
Blood sugar issues
Consuming high levels of caffeine and sugar can cause hypoglycaemia, which can trigger symptoms of anxiety, mood swings, and impaired cognitive function.Lake, J. (2009). Integrative Mental Health Care. New York, NY: W.W. Norton & Co., p. 263.
Homocysteine levels
Research suggests that alcohol consumption can increase homocysteine levels, which are associated with heart disease.Bleich, S., Bleich, K., Kropp, S., Bittermann, H.-J., Degner, D., Sperling, W., Rüther, E., Kornhuber, J. (2001). Moderate alcohol consumption in social drinkers raises plasma homocysteine levels: a contradiction to the “French Paradox”?’ Alcohol and Alcoholism, 36(3), pp. 189–192.
Mental health effects of common addictive substances
Different addictive substances can affect our minds and bodies in different ways.
Three of the most common, especially in affluent Western society, are caffeine, alcohol, and recreational drugs.
Caffeine is a stimulant, which is why drinking a cup of coffee or a caffeinated soda gives us a temporary surge of energy. Coffee is also full of antioxidants, and can have a healthy impact on the brain.
Drinking caffeine to excess, however, can cause symptoms such as:
- Anxiety
- Panic
- Sleep issues
Caffeine addiction can then lead to withdrawal symptoms, including:
- Headaches
- Sleepiness
- Irritability
- Depression
- A lack of concentration
Some people can consume a lot of coffee without showing any ill effects.
In the case of caffeinated sodas, however, the sugar they contain may also be detrimental to our mental health, so it can be doubly damaging.
While at first it has a calming, relaxing effect, alcohol can subsequently increase our levels of cortisol (the stress hormone), leading to anxiety, and it often has a depressive effect as well.
Severe cases of alcohol intoxication and/or withdrawal can cause symptoms that are ‘sometimes mistakenly interpreted as a primary psychiatric or medical disorder’:Lake, J. (2009). Integrative Mental Health Care. New York. NY: W.W. Norton & Co., p. 260.
- Severe anxiety
- Insomnia
- Violent mood swings
- Cognitive impairment
- Psychosis
These symptoms may put a strain on relationships with family and friends, and can often interfere with the individual’s ability to function at work.
Alcohol can also cause nutritional imbalances, neurotransmitter imbalances, and blood sugar issues. Being a toxic substance, there are numerous ways in which it can damage our bodies:Perlmutter, D., Colman, C. (2004). The Better Brain Book. New York, NY: Riverhead Books, p. 27.
- It dehydrates our bodies generally, damaging our skin and the ability of our brains to function
- The toxic chemicals it contains cause free radicals, which can damage the membranes in the brain
- More than four units of alcohol inhibits detoxification, and puts a heavy burden on the liver
Most recreational drugs are damaging to our brain chemistry, and cause severe imbalances in neurotransmitters, which can lead to:
- Anxiety and panic
- Depression
- Irritability
- Poor memory
- Poor concentration and attention
- Psychosis
- Sleep issues
Recreational drugs can be highly addictive, sometimes causing addiction after only a single use, and once someone is addicted to them, it can become extremely difficult to stop taking them.
Depending on the substance used and the biochemistry of the user, taking recreational drugs may also prove fatal, whether after a period of chronic use or even a single use (through an overdose or a ‘bad reaction’).
Mental health as a contributor to addiction
While addiction is a key contributor to mental health issues, those issues can often be contributors to addiction too.
There is no one factor alone which can cause or prevent addiction. It’s the result of a combination of factors, which include stress, trauma, genetic disposition, biochemical imbalances, and more.Sheff, D. (2014) Clean. New York, NY: Mariner, p. xi.
There is usually a strong link between mental health issues and addiction. People with undiagnosed or untreated mental health issues often want to alleviate their symptoms, or distract themselves, and may try to self-medicate with addictive substances and/or behaviours.
Those with depression, anxiety, poor concentration and attention, poor memory and insomnia may try to escape the discomfort of their condition through the repeated use of substances and behaviours.
Two good examples of this are autism/Asperger syndrome, and Attention Deficit Hyperactivity Disorder (ADHD). They are often interconnected:
- Between 30% and 50% of autistic people have symptoms of ADHD
- Two-thirds of people with ADHD show autistic traits
People with Asperger syndrome and autism are predisposed to over-learning, and so their repetitive habits can become more deeply rooted over time.
They may use addictive substances or behaviours to alleviate their symptoms, which can include:
- Oversensitivity
- Social anxiety
- Difficulty connecting with others
- Depressive tendencies
- An inability to regulate emotions and behaviour
A primary symptom of ADHD is impulsivity, and impulsive behaviour is often associated with drug use. Around 20% of people who abuse narcotics have ADHD, at least four times higher than that seen in the general population.Szalavitz, M. (2016). Unbroken Brain. New York: Picador, p. 54.
ADHD has also been shown to be a significant risk factor when combined with nicotine and alcohol consumption.Ohlmeier, M., Peters, K., Kordon, A., Seifert, J., Te Wildt, B., Wiese, B., Ziegenbein, M., Emrich, H. and Schneider, U. (2007). Nicotine And Alcohol Dependence In Patients With Comorbid Attention-Deficit/Hyperactivity Disorder (ADHD). Alcohol and Alcoholism, 42(6), 539–543. Available at: https://pdfs.semanticscholar.org/422b/2a5b3137e13e3b72f27d507623bbe58fde2a.pdf [Accessed July 2016].
Other symptoms of untreated ADHD include:
People struggling with undiagnosed ADHD may resort to self-medication in an attempt to manage these symptoms. For example, they may use addictive substances in an attempt to:
- Slow themselves down (hyperactivity)
- Aid their sleep (insomnia)
- Boost their mood (depression)
This use can quickly turn into dependence.
It is worth noting, however, that the risks of dependence are often overstated. For instance, the prescription of stimulant drugs to treat ADHD has been blamed in the media for drug addiction. But one long-term study, which followed one hundred boys with ADHD for ten years, showed no increased risk of substance abuse in the boys who took medication.Molina, B., Pelham, W. (2014.) ‘Attention-Deficit Hyperactivity Disorder and risk of substance use disorder’. Annual Review of Psychology, 10, pp. 607–639.
Other contributors to addiction
Many addictive substances are legal and readily available, such as alcohol, cigarettes, and prescription medication. Some people can use them at various intervals and never become addicted, while others can develop an addiction after only a single use. We all have different levels of tolerance.
Most of us do not become addicted to these types of substance:
- In the U.S., the National Institute on Alcohol Abuse and Alcoholism has estimated that ‘87% of adult Americans drink, yet 87% of Americans are not alcoholics’.Grace, A. (2015). This Naked Mind: Control Alcohol, Find Freedom, Rediscover Happiness and Change Your Life. ASPN Publications, p. 40.
- In fact, only ’10 to 20%’ of people who try even ‘the most stigmatised drugs like heroin, crack, and methamphetamine’ end up addicted to them.Szalavitz, M. (2016). Unbroken Brain. New York, NY: Picador, p. 4.
But when someone does have a tendency towards addiction, occasional use can swiftly become habitual.
Some factors in our propensity to become addicted include:
There is no single ‘gene for addiction’, but addiction does tend to run in families. Research has shown that:Enoch, M.A., Goldman, D. (2001). ‘The genetics of alcoholism and alcohol abuse’. Current Psychiatry Reports, 3(2), p. 144–151.
- The children of drug and alcohol addicts are eight times more likely to develop an addiction
- If those children also experience a traumatic childhood, they are at even greater risk of going on to become addicted
But even if someone has a genetic predisposition to addiction, the genetic heritability of addiction ranges between 40–60%, which leaves a lot of scope for environmental factors and lifestyle decisions.Szalavitz, M. (2016). Unbroken Brain. New York, NY: Picador, p. 63.
An exposure to addictive substances during our childhood or adolescence increases the risk of developing addiction. The brain is still developing, and therefore more vulnerable to addictive substances and patterns.Szalavitz, M. (2016). Unbroken Brain. New York, NY: Picador, p.38.Szalavitz, M. (2016). Unbroken Brain. New York, NY: Picador, p.4.Dupuy, J. (2013). Integral Recovery. Albany, NY: State University of New York Press, p. 3.
- The odds of becoming an alcoholic for those who start drinking aged 14 or younger are nearly 50%, while at the age of 21 or more, that goes down to 9%
- The risk of becoming addicted to marijuana, cocaine, or benzodiazepines is two to four times higher for those who take them aged 11 to 17, compared to those who start taking them aged 18 or more
- 90% of all substance addictions start in adolescence, and most illegal drug addictions end by the age of 30
- Young people are much more susceptible to becoming addicted; for over a decade now, 12- to 17-year-olds have labelled drugs the greatest problem they face in a survey by Columbia University’s National Center on Addiction and Substance Abuse
It is also in adolescence that we develop our main coping strategies and behavioural patterns for our adult lives. Drug and alcohol use can interfere with this process:Arain, M., Haque, M., Johal, L., Mathur, P., Nel, W., Rais, A., Sandhu, R., Sharma, S. (2013). ‘Maturation of the adolescent brain’. Neuropsychiatric Disease and Treatment, 9: 449–461.
- In adolescent brains, the judgement and control areas of the frontal lobes don’t finish maturing until the age of 25
- Addiction is far less common in people who use drugs for the first time after the same age, and it often remits with or without treatment in the mid-20s
- During adolescence the limbic system develops ahead of the control systems described above; it drives us towards immediate gratification, risk-taking, excitement, and danger, all of which are connected to substance use
Psychological trauma, particularly in childhood, can be a major contributor to addiction.
Adverse childhood experiences may include:
- Being neglected
- Suffering emotional, physical, and sexual abuse
- Living in a house with domestic violence
- Having a mentally ill or addicted parent
- Having a parent in prison
- Losing a parent to divorce or death
The Adverse Childhood Experiences (ACE) study, which included some 17,000 participants in California’s Kaiser Permanente insurance program, found multiple relationships between severe childhood stress and many types of addiction.Kim, V. (2017). ‘The link between opioid misuse and childhood trauma’. The Fix. [online] Available at: https://www.thefix.com/link-between-opioid-misuse-and-childhood-trauma [2 Nov. 2017].
Heroin users provide an especially clear example of this relationship:Szalavitz, M. (2016). Unbroken Brain. New York, NY: Picador, p. 65.
- Half of all heroin addicts have suffered emotional and physical neglect, leading one research group to characterise the typical addiction experience as a ‘shattered childhood’
- Between one-third and half of all heroin injectors have experienced sexual abuse, with women having approximately double the amount of sexual abuse rates than those for men
- In 50% of those sexual abuse cases, the offence was not just a single incident but an ongoing series of attacks, typically conducted by a relative or family friend
Someone going through a very difficult time, involving trauma, relationship difficulties, or tough socio-economic circumstances, may become addicted when under more favourable circumstances they would not.
When we become addicted to a substance or behaviour, it’s usually because that substance or behaviour is fulfilling an unmet psycho-spiritual need, at least in the short term. For instance, it might:
- Deflect or numb our pain, or other unpleasant feelings such as fear, anxiety, and loneliness
- Help us escape from our current situation
- Compensate for our feelings of emptiness, or our lack of purpose
While in the short term the substance or behaviour can make us feel better, in the long term it can make us feel much worse, and have a negative impact on our mental health.
Read more about how life circumstances can impact our mental health by clicking on the links below:
Some argue that being exposed to addictive substances can turn anyone into an addict, and that repeated exposure increases the likelihood of addiction.Grace, A. (2015). This Naked Mind: Control Alcohol, Find Freedom, Rediscover Happiness and Change Your Life. ASPN Publications, p. 42.
This is because several of these substances are chemically addictive, including:
- Alcohol
- Tobacco
- Recreational drugs
- Certain prescription medications
When we consume them, the brain releases neurotransmitters such as serotonin and dopamine, which can lead to feelings of pleasure and relaxation but also cause cravings for more. The more we use the substance, the more our tolerance to it may increase, meaning that we need a greater amount of it to give us the same ‘good’ feeling.
Certain biochemical imbalances can predispose us towards addiction. This can include:
- Hormonal imbalances
- Nutritional imbalances
- Blood sugar imbalances
- Excessive toxicity
- Gut issues, such as leaky gut
Our brain regulates the levels of hormones in our bodies, and when it detects an imbalance it triggers hormone production. This can have the side-effect of mental health symptoms, and these make us vulnerable to addictive behaviour or substances.Sat Dharam Kaur. (2016). ‘The Gut, the Brain and Addiction’. Beyond Addiction. [online] Available at: http://beyondaddiction.ca/2016/09/04/gut-brain-addiction/ [accessed 2 Nov. 2017].
The nutritional deficiencies resulting from addiction can also make recovery harder. If we aren’t digesting and absorbing sufficient nutrients, our brains won’t trigger the correct neurotransmitters and hormones.
Kathleen DesMaisons has argued that people who suffer from ‘sugar sensitivity’ are especially prone to addiction. When they consume carbohydrates, an extremely powerful blood-sugar response can be triggered, releasing opioids and dopamine in their brains and giving feelings of pleasure. People with this nutritional imbalance, she suggests, are prone to a sugar addiction that, if left untreated, ‘can open the gate to other addictions’.DesMaisons, K. (2008). Potatoes Not Prozac. New York, NY: Simon & Schuster, p. 3.
A lifestyle that exposes us to addictive substances can eventually lead to addiction, when it’s combined with unhealthy habits. These could include, for example:
Our modern Western lifestyles also emphasise material gain and success. As a result, when people are poor or unsuccessful, they may feel inadequate or seek pleasure wherever they can, and this need to ‘fill the void’ can lead to substance abuse.
As the Jungian psychologist Robert Johnson makes clear: ‘Addiction is nothing other than a severely degraded substitute for the true experience of joy’.In Chopra, D. (1997). Overcoming Addictions. New York, NY: Harmony Books, p. 6.
Through a combination of genetic, biochemical, and psycho-spiritual factors, certain people may have a personality more prone to addiction than others.
The ‘Addictive Personality’ model argues that this is the case: some people are born with inherently addictive personalities, and if these people are exposed to addictive substances, they will become addicts.Jampolsky, L. (2008). Healing The Addictive Personality. Berkeley, CA: Celestial Arts, p. 4.
But, while some character traits are traditionally associated with addiction, to view it as an inherent part of someone’s personality can disempower that person, by assuming that their addiction is inevitable.
Instead, we can imagine the Addictive Personality as a mindset, or set of behaviours, that makes the person more vulnerable to addiction. These might include:
- Perfectionism
- People-pleasing
- Extroversion
- Impulsivity
- Recklessness
- Social anxiety
- Depression