Mitochondrial dysfunction
You may not know much about mitochondria, or that they play a key role in your mental health.
But these tiny organelles, which are an essential part of every one of our cells, and provide them with the energy to function via adenosine triphosphate (ATP), play a vital role in our brain and mental health.
Dysfunctional mitochondria could be contributing to mental health symptoms such as depression, anxiety, poor memory, poor concentration and attention, insomnia, and neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease.
Mitochondria 101
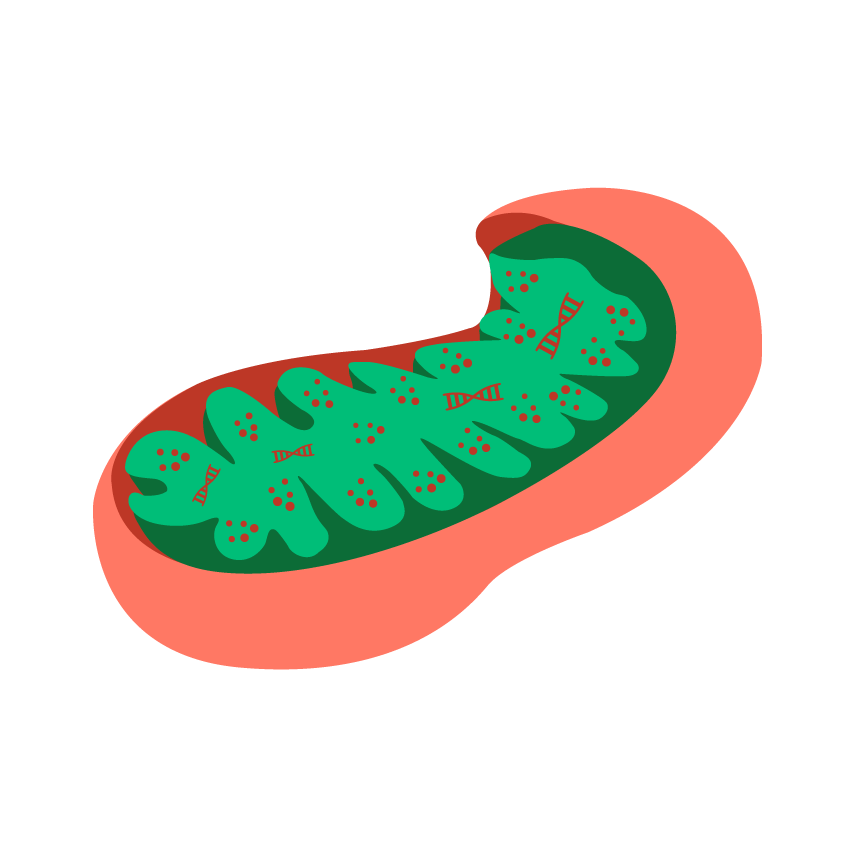
Mitochondria are tiny organelles inside each of our trillions of cells, and they function like the batteries of each cell, producing ATP energy to power the cell’s function.
Our metabolism, hormones, central nervous system, and all our organs are powered by mitochondrial energy.
Most cells have thousands of mitochondria powering them. For example liver cells have between 400 and 4,000 and heart cells have roughly 6,000 mitochondria.Huang, X., Sun, L., Ji, S., Zhao, T., Zhang, W., Xu, J., Zhang, J., Wang, Y., Wang, X., Franzini-Armstrong, C., Zheng, M., & Cheng, H. (2013). Kissing and nanotunneling mediate intermitochondrial communication in the heart. Proceedings of the National Academy of Sciences of the United States of America, 110(8), 2846–2851. https://doi.org/10.1073/pnas.1300741110, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3581932/ [accessed 2nd November 2020] Hossain, M. G., Akter, S., Ohsaki, E., & Ueda, K. (2020). Impact of the Interaction of Hepatitis B Virus with Mitochondria and Associated Proteins. Viruses, 12(2), 175. https://doi.org/10.3390/v12020175, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7077294/ [accessed 2nd November 2020]
Mitochondria need two things to produce energy: food (glucose, fat or protein) and oxygen.
Interestingly, the Chinese character for Qi (vital energy) is rice (glucose) and air (oxygen). In Western science, the closest thing to the Qi of Chinese medicine, and the Prana of Ayurvedic medicine, is Mitochondrial energy.
Mitochondria evolved from bacteria, and have their own DNA, called mitochondrial DNA (mtDNA). Mitochondria provide not just more energy for their host cells, but importantly, more energy per gene.Lane, N., & Martin, W. F. (2015). Eukaryotes really are special, and mitochondria are why. Proceedings of the National Academy of Sciences of the United States of America, 112(35), E4823. https://doi.org/10.1073/pnas.1509237112, https://pubmed.ncbi.nlm.nih.gov/26283405/ [accessed 2nd November 2020] Evolution of complex life requires a lot of energy to build and maintain this complexity. Mitochondria power genes to allow complex life to not just survive, but to adapt and thrive in an ever changing world.
Mitochondria have a shelf life of days for most tissue, and are designed to self-regulate, which means that when they are old, infirm or dysfunctional, they initiate mitophagy – which effectively means “mitochondrial digestion”. This is a natural process that is needed as a form of quality control to ensure mitochondria can continue to give our brain and body optimum levels of ATP.
Another part of mitochondrial quality control (or mitochondrial dynamics) is fusion and fission where mitochondria continually fuse and divide to ‘weed out’ worn out mitochondrial components which are ready for mitophagy.Griffiths, R., 2018. Mitochondria in Health and Disease: Personalized Nutrition for Healthcare Practitioners. Singing Dragon.
Mitochondria and the brain
Neurons within our brain require substantially more mitochondria than the rest of the body, due to their incredibly high energy needs.
For example, Some dopamine producing neurons have been estimated to require as many as 1 million mitochondria.Misgeld, T., & Schwarz, T. L. (2017). Mitostasis in Neurons: Maintaining Mitochondria in an Extended Cellular Architecture. Neuron, 96(3), 651–666. https://doi.org/10.1016/j.neuron.2017.09.055, https://pubmed.ncbi.nlm.nih.gov/29096078/ [accessed 2nd November 2020] Even though the brain makes up only 2% of our body weight, the trillions of mitochondria that the brain contains result in up to 20% of our oxygen and 25% of our total glucose being consumed by these hungry brain organelles.Pei, L., & Wallace, D. C. (2018). Mitochondrial Etiology of Neuropsychiatric Disorders. Biological psychiatry, 83(9), 722–730. https://doi.org/10.1016/j.biopsych.2017.11.018, https://pubmed.ncbi.nlm.nih.gov/29290371/ [accessed 2nd November 2020]
Healthy mitochondria which are both abundant and functional, are necessary to produce sufficient amounts of ATP for optimal brain function and mental health.
How mitochondria can become dysfunctional
Mitochondria can become dysfunctional through excess stress, inflammation, obesity, poor diet, excessive toxins and a sedentary lifestyle.Kaplan, B. J., Rucklidge, J. J., Romijn, A., & McLeod, K. (2015). The Emerging Field of Nutritional Mental Health: Inflammation, the Microbiome, Oxidative Stress, and Mitochondrial Function. Clinical Psychological Science, 3(6), 964–980. https://doi.org/10.1177/2167702614555413, https://journals.sagepub.com/doi/abs/10.1177/2167702614555413 [accessed 2nd November 2020] See below for more detail on root causes of mitochondrial dysfunction.
Dysfunctional mitochondria not only fail to produce enough ATP for optimal cell power, but also produce high levels of damaging ROS (Reactive Oxygen Species).
If left unchecked, excessively damaged and dysfunctional mitochondria can act as cell saboteurs and signal the whole cell to commit suicide in a process called apoptosis (programmed cell death).Griffiths, R., 2018. Mitochondria in Health and Disease: Personalized Nutrition for Healthcare Practitioners. Singing Dragon. Apoptosis is a natural process designed to protect old and dysfunctional cells, however it needs to be carefully regulated. Excessively damaged mitochondria can lead to excessive apoptosis.
How dysfunctional mitochondria affect mental health
People with depression have been shown to have impaired CNS (central nervous system) energy production, impaired neurotransmitter production, and reduced neurotrophic factors such as BDNF (brain derived neurotrophic factor) and NGF (nerve growth factor) which are essential for neural plasticity.Yang, T., Nie, Z., Shu, H., Kuang, Y., Chen, X., Cheng, J., Yu, S., & Liu, H. (2020). The Role of BDNF on Neural Plasticity in Depression. Frontiers in cellular neuroscience, 14, 82. https://doi.org/10.3389/fncel.2020.00082, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7174655/ [Accessed 2nd November 2020] Markham, A., Bains, R., Franklin, P., & Spedding, M. (2014). Changes in mitochondrial function are pivotal in neurodegenerative and psychiatric disorders: how important is BDNF?. British journal of pharmacology, 171(8), 2206–2229. https://doi.org/10.1111/bph.12531, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3976631/ [Accessed 2nd November 2020]
Neural plasticity can be defined as the way an individual remodels their inner neural connections according to their outer environment. Insufficient or inappropriate neural plasticity may leave an individual mentally ill-equipped to thrive in their surrounding environment.Allen, J., Romay-Tallon, R., Brymer, K. J., Caruncho, H. J., & Kalynchuk, L. E. (2018). Mitochondria and Mood: Mitochondrial Dysfunction as a Key Player in the Manifestation of Depression. Frontiers in neuroscience, 12, 386. https://doi.org/10.3389/fnins.2018.00386, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5997778/ [accessed 2nd November 2020]
Impaired or dysfunctional mitochondria, dysfunctional mitophagy and excessive apoptosis are implicated in the pathology of Alzheimer’s disease and other neurological and mental health disorders.Allen, J., Romay-Tallon, R., Brymer, K. J., Caruncho, H. J., & Kalynchuk, L. E. (2018). Mitochondria and Mood: Mitochondrial Dysfunction as a Key Player in the Manifestation of Depression. Frontiers in neuroscience, 12, 386. https://doi.org/10.3389/fnins.2018.00386, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5997778/ [accessed 2nd November 2020] Cabral-Costa, J. and Kowaltowski, A., 2020. Neurological Disorders And Mitochondria. [online] ScienceDirect. Available at: <https://www.sciencedirect.com/science/article/pii/S0098299719301001> [Accessed 2nd November 2020]
Dysfunctional mitochondria can lead to:
- ATP is necessary for axon and neuron growth, and BDNF (Brain Derived Neurotrophic Factor) assists this growth by improving mitochondrial efficiency to increase neuronal ATPMarkham, A., Bains, R., Franklin, P., & Spedding, M. (2014). Changes in mitochondrial function are pivotal in neurodegenerative and psychiatric disorders: how important is BDNF?. British journal of pharmacology, 171(8), 2206–2229. https://doi.org/10.1111/bph.12531, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3976631/ [accessed 2nd November 2020]
- when ATP production is compromised by dysfunctional or reduced numbers of mitochondria, there is decreased synaptic plasticityMarkham, A., Bains, R., Franklin, P., & Spedding, M. (2014). Changes in mitochondrial function are pivotal in neurodegenerative and psychiatric disorders: how important is BDNF?. British journal of pharmacology, 171(8), 2206–2229. https://doi.org/10.1111/bph.12531, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3976631/ [accessed 2nd November 2020]
- mitochondria enable neurogenesis (increased brain plasticity and regrowth) by supporting the process of maturation from stem cell to neuron, and by accumulating at the site of axon growth to provide vital ATPNiklison-Chirou, M. V., Agostini, M., Amelio, I., & Melino, G. (2020). Regulation of Adult Neurogenesis in Mammalian Brain. International journal of molecular sciences, 21(14), 4869. https://doi.org/10.3390/ijms21144869, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7402357/ [accessed 2nd November 2020]
- NGF (Nerve Growth Factor) is required to allow for this mitochondrial accumulation
- depressed patients have been found to have either low or dysregulated levels of NGF and BDNFMondal, A. C., & Fatima, M. (2019). Direct and indirect evidences of BDNF and NGF as key modulators in depression: role of antidepressants treatment. The International journal of neuroscience, 129(3), 283–296. https://doi.org/10.1080/00207454.2018.1527328, https://pubmed.ncbi.nlm.nih.gov/30235967/ [accessed 2nd November 2020]
- the natural byproduct of mitochondrial energy production is ROS (Reactive Oxygen Species)
- in small amounts ROS are vital to our mental and physical wellbeing by triggering our DNA to manufacture many anti-ageing antioxidantsNunn, A.V., Guy, G.W. and Bell, J.D. (2015). Hormesis and Cognitive Function. In Diet and Exercise in Cognitive Function and Neurological Diseases (eds T. Farooqui and A.A. Farooqui). doi:10.1002/9781118840634.ch13, https://onlinelibrary.wiley.com/doi/abs/10.1002/9781118840634.ch13 [accessed 2nd November 2020]
- excessive amounts of ROS however can undermine the enzymes and cofactors involved in the synthesis of monoamine neurotransmitters which support mental health, such as serotonin, dopamine, and noradrenalineRawdin, B. J., Mellon, S. H., Dhabhar, F. S., Epel, E. S., Puterman, E., Su, Y., Burke, H. M., Reus, V. I., Rosser, R., Hamilton, S. P., Nelson, J. C., & Wolkowitz, O. M. (2013). Dysregulated relationship of inflammation and oxidative stress in major depression. Brain, behavior, and immunity, 31, 143–152. https://doi.org/10.1016/j.bbi.2012.11.011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3669232/ [accessed 2nd November 2020]
- as we age, the activity of monoamine oxidase enzymes increases, further degrading monoamine neurotransmittersDuncan, J., Johnson, S., & Ou, X. M. (2012). Monoamine oxidases in major depressive disorder and alcoholism. Drug discoveries & therapeutics, 6(3), 112–122., https://pubmed.ncbi.nlm.nih.gov/22890201/ [accessed 2nd November 2020]
- StressCalcia, M. A., Bonsall, D. R., Bloomfield, P. S., Selvaraj, S., Barichello, T., & Howes, O. D. (2016). Stress and neuroinflammation: a systematic review of the effects of stress on microglia and the implications for mental illness. Psychopharmacology, 233(9), 1637–1650. https://doi.org/10.1007/s00213-016-4218-9, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4828495/ [accessed 2nd November 2020], traumaDanese, A., & J Lewis, S. (2017). Psychoneuroimmunology of Early-Life Stress: The Hidden Wounds of Childhood Trauma?. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology, 42(1), 99–114. https://doi.org/10.1038/npp.2016.198, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5143500/ [accessed 2nd November 2020], obesityGuillemot-Legris, O., & Muccioli, G. G. (2017). Obesity-Induced Neuroinflammation: Beyond the Hypothalamus. Trends in neurosciences, 40(4), 237–253. https://doi.org/10.1016/j.tins.2017.02.005, https://pubmed.ncbi.nlm.nih.gov/28318543/ [accessed 2nd November 2020], poor dietCai D. (2013). Neuroinflammation and neurodegeneration in overnutrition-induced diseases. Trends in endocrinology and metabolism: TEM, 24(1), 40–47. https://doi.org/10.1016/j.tem.2012.11.003, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3556486/ [accessed 2nd November 2020], sedentary lifestyleSpielman, L. J., Little, J. P., & Klegeris, A. (2016). Physical activity and exercise attenuate neuroinflammation in neurological diseases. Brain research bulletin, 125, 19–29. https://doi.org/10.1016/j.brainresbull.2016.03.012, https://pubmed.ncbi.nlm.nih.gov/27021169/ [accessed 2nd November 2020], brain injuryXiong, Y., Mahmood, A., & Chopp, M. (2018). Current understanding of neuroinflammation after traumatic brain injury and cell-based therapeutic opportunities. Chinese journal of traumatology = Zhonghua chuang shang za zhi, 21(3), 137–151. https://doi.org/10.1016/j.cjtee.2018.02.003, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6034172/ [accessed 2nd November 2020], gut dysbiosisClapp, M., Aurora, N., Herrera, L., Bhatia, M., Wilen, E., & Wakefield, S. (2017). Gut microbiota’s effect on mental health: The gut-brain axis. Clinics and practice, 7(4), 987. https://doi.org/10.4081/cp.2017.987, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/ [accessed 2nd November 2020], toxins and peripheral inflammationChang, E. H., Chavan, S. S., & Pavlov, V. A. (2019). Cholinergic Control of Inflammation, Metabolic Dysfunction, and Cognitive Impairment in Obesity-Associated Disorders: Mechanisms and Novel Therapeutic Opportunities. Frontiers in neuroscience, 13, 263. https://doi.org/10.3389/fnins.2019.00263, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6460483/ [accessed 2nd November 2020], can all lead to CNS inflammation known as neuroinflammation
- mitochondria are both sources and targets of excess ROS during the above health challenges which can cause further neuroinflammation, leading to an increased risk of depressionCaruso, G., Benatti, C., Blom, J., Caraci, F., & Tascedda, F. (2019). The Many Faces of Mitochondrial Dysfunction in Depression: From Pathology to Treatment. Frontiers in pharmacology, 10, 995. https://doi.org/10.3389/fphar.2019.00995, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6746908/ [accessed 2nd November 2020], anxietyBurroughs, S. and French, D., 2020. Depression And Anxiety: Role Of Mitochondria. [online] ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S0953711207000245 [Accessed 6th November 2020], insomniaGulec, M., Ozkol, H., Selvi, Y., Tuluce, Y., Aydin, A., Besiroglu, L., & Ozdemir, P. G. (2012). Oxidative stress in patients with primary insomnia. Progress in neuro-psychopharmacology & biological psychiatry, 37(2), 247–251. https://doi.org/10.1016/j.pnpbp.2012.02.011, https://pubmed.ncbi.nlm.nih.gov/22401887/ [accessed 2nd November 2020], poor memoryLin, T., Liu, G. A., Perez, E., Rainer, R. D., Febo, M., Cruz-Almeida, Y., & Ebner, N. C. (2018). Systemic Inflammation Mediates Age-Related Cognitive Deficits. Frontiers in aging neuroscience, 10, 236. https://doi.org/10.3389/fnagi.2018.00236, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6088306/ [accessed 2nd November 2020], and other mental health issues
- mitochondria play a role in inflammation and growth of tissue and immune cells
- when mitochondria are in anabolic/proinflammatory mode (under threat) within microglia (resident immune cells of the Central Nervous System, or CNS) they produce ROS instead of ATPCulmsee, C., Michels, S., Scheu, S., Arolt, V., Dannlowski, U., & Alferink, J. (2019). Mitochondria, Microglia, and the Immune System-How Are They Linked in Affective Disorders?. Frontiers in psychiatry, 9, 739. https://doi.org/10.3389/fpsyt.2018.00739, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6333629/ [accessed 2nd November 2020]
- in this mode BDNF levels fall and undermine neural plasticity and neurogenesisPatterson S. L. (2015). Immune dysregulation and cognitive vulnerability in the aging brain: Interactions of microglia, IL-1β, BDNF and synaptic plasticity. Neuropharmacology, 96(Pt A), 11–18. https://doi.org/10.1016/j.neuropharm.2014.12.020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4475415/ [accessed 2nd November 2020] Zhang, L., Zhang, J., & You, Z. (2018). Switching of the Microglial Activation Phenotype Is a Possible Treatment for Depression Disorder. Frontiers in cellular neuroscience, 12, 306. https://doi.org/10.3389/fncel.2018.00306, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6232769/ [accessed 2nd November 2020]
- chronic activation of microglia can lead to the death of neurons due to excessive apoptosis
- apoptosis is a mitochondria dependent processVisentin, A., Colombo, R., Scotton, E., Fracasso, D. S., da Rosa, A. R., Branco, C. S., & Salvador, M. (2020). Targeting Inflammatory-Mitochondrial Response in Major Depression: Current Evidence and Further Challenges. Oxidative medicine and cellular longevity, 2020, 2972968. https://doi.org/10.1155/2020/2972968, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7178465/ [accessed 2nd November 2020]
What causes mitochondrial dysfunction?
In a word, “stress”, both too much and too little!
Stress is a call to the body for more energy and resources. In appropriate amounts, stress can be enlivening and leads us to be more resilient against future stresses.
Mitochondria, like the rest of our body, thrive on small amounts of challenge and stress. This is known as hormesis. Examples of hormesis are exercise, plant polyphenols, extreme heat or cold — all of which in small doses are stimulating and healthy for the mitochondria, triggering our body’s own antioxidant response. ROS generated during beneficial stress are signals for the body to boost protective measures.
When stress is excessive however, the call for energy and resources exceed the body’s psychological, biochemical and energetic reserves, leading to a decline in health and wellbeing.Turkson, S., Kloster, A., Hamilton, P. J., & Neigh, G. N. (2019). Neuroendocrine drivers of risk and resilience: The influence of metabolism & mitochondria. Frontiers in neuroendocrinology, 54, 100770. https://doi.org/10.1016/j.yfrne.2019.100770, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6886586/ [accessed 2nd November 2020] Burroughs, S. and French, D., 2020. Depression And Anxiety: Role Of Mitochondria. [online] ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S0953711207000245 [Accessed 6th November 2020]
Mitochondria are sensitive to our environment, and, much like us, are designed to respond to states of threat or safety. Robert Naviaux coined the term “cell danger response” which is when our cells launch a biochemical chain reaction in response to stressors, sometimes continuing to do so even when the threat has passed.Naviaux R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16, 7–17. https://doi.org/10.1016/j.mito.2013.08.006, https://pubmed.ncbi.nlm.nih.gov/23981537/ [accessed 2nd November 2020]
Peace time metabolism versus defense mode
When not presented with excessive stressors, our mitochondria are in “peace time metabolism” (a term coined by Ari Whitten of The Energy Blueprint).
Peace time metabolism
- mitochondria produce energy (ATP)
- they are in aerobic/catabolic (breakdown) mode
- they limit excessive tissue growth and reduce inflammation
However, when presented with too many stressors and energy demands, our mitochondria feel under threat and shift into “defense mode”.
Defense mode
- mitochondria stop producing energy
- they produce excessive levels of ROS (reactive oxygen species), which are oxidants
- they are in anaerobic/anabolic (build-up) mode
- this promotes tissue growth/proliferation (it can lead to the proliferation of cancerous cells for instance) and inflammation
This response is designed to protect us in the short term, however when it gets stuck on ON (as in the cell danger response) it can lead to uncontrolled cell proliferation and chronic inflammation.Griffiths, R., 2018. Mitochondria in Health and Disease: Personalized Nutrition for Healthcare Practitioners. Singing Dragon.
Unresolved chronic inflammation can lead to too much apoptosis (programmed cell death) in the case of neurons and brain health, and too little apoptosis in the case of cancer.Elmore S. (2007). Apoptosis: a review of programmed cell death. Toxicologic pathology, 35(4), 495–516. https://doi.org/10.1080/01926230701320337, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2117903/ [accessed 2nd November 2020]
Ideally “defense mode” for mitochondria should be stood down as soon as a threat or demand has passed.
Excessive stress (psychological and oxidative stress) can tip mitochondria from peace time metabolism when they produce energy, to defense mode when they cause cell proliferation and inflammation.
The stressors that cause mitochondrial dysfunction
As we have seen, excessive stress can damage mitochondria. When cells get stuck in “defense mode” due to chronic and excessive stressors (be they from biochemical, psychological, or behavioural sources as listed below), it can lead to neuroinflammation in response to perceived threat.
- neurons, their blood supply and the CNS immune system all work as a ‘tight knit’ system called the “neurovascular unit”
- excessive stress can undermine the neurovascular unit and promote neuroinflammationNajjar, S., Pearlman, D. M., Devinsky, O., Najjar, A., & Zagzag, D. (2013). Neurovascular unit dysfunction with blood-brain barrier hyperpermeability contributes to major depressive disorder: a review of clinical and experimental evidence. Journal of neuroinflammation, 10, 142. https://doi.org/10.1186/1742-2094-10-142, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4220803/ [accessed 2nd November 2020]
- with excessive stress too many demands are made of our mitochondria and energy metabolism, exceeding our ability to produce it, which leads to high levels of ROS (reactive oxygen species) and RNS (reactive nitrogen species)
- these can damage mitochondrial DNA (mtDNA)
- small amounts of ROS are protective through mitohormesis (hormesis to the mitochondria), but large amounts can be extremely damagingTurkson, S., Kloster, A., Hamilton, P. J., & Neigh, G. N. (2019). Neuroendocrine drivers of risk and resilience: The influence of metabolism & mitochondria. Frontiers in neuroendocrinology, 54, 100770. https://doi.org/10.1016/j.yfrne.2019.100770, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6886586/ [accessed 2nd November 2020] Radi R. (2018). Oxygen radicals, nitric oxide, and peroxynitrite: Redox pathways in molecular medicine. Proceedings of the National Academy of Sciences of the United States of America, 115(23), 5839–5848. https://doi.org/10.1073/pnas.1804932115, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6003358/ [accessed 2nd November 2020]
- mitochondrial DNA (mtDNA) is relatively unprotected compared to cell nucleus DNA, and is easily damagedXie, M., Doetsch, P. W., & Deng, X. (2015). Bcl2 inhibition of mitochondrial DNA repair. BMC cancer, 15, 586. https://doi.org/10.1186/s12885-015-1594-1, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4535531/ [accessed 2nd November 2020]
- this damage to mtDNA further increases free radicals and causes ageing and degeneration, as mitochondria can’t make enough ATP for their host cells
- these dysfunctional mitochondria are usually removed through a process called mitophagy, however, high levels of mitochondrial damage can lead a cell to self-destruct (apoptosis)
- stressed mitochondria release mtDNA and cardiolipin (a type of fat only found only in mitochondria and bacteria) into the cytosol
- once outside mitochondria, these internal mitochondrial components activate the inflammasome, triggering a strong inflammatory responseKauppinen A. (2018) Mitochondria-Associated Inflammasome Activation and Its Impact on Aging and Age-Related Diseases. In: Fulop T., Franceschi C., Hirokawa K., Pawelec G. (eds) Handbook of Immunosenescence. Springer, Cham. https://doi.org/10.1007/978-3-319-64597-1_107-1, https://link.springer.com/referenceworkentry/10.1007%2F978-3-319-64597-1_107-1 [accessed 2nd November 2020]
mtDNA can be detected in blood plasma of depressive patients and suicide attempters, indicating that stress, mitochondrial dysfunction and neuropathology are all deeply interconnected.Lindqvist, D., Wolkowitz, O. M., Picard, M., Ohlsson, L., Bersani, F. S., Fernström, J., Westrin, Å., Hough, C. M., Lin, J., Reus, V. I., Epel, E. S., & Mellon, S. H. (2018). Circulating cell-free mitochondrial DNA, but not leukocyte mitochondrial DNA copy number, is elevated in major depressive disorder. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology, 43(7), 1557–1564. https://doi.org/10.1038/s41386-017-0001-9, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5983469/ [accessed 2nd November 2020]
Stressors to mitochondria can be biochemical, psychological, or lifestyle/behavioural:
It is the dual role of mitochondria as energy providers (catabolic mode) or suppliers of cell components (anabolic mode) which underlies a large part of how diet translates into health or disease.
The typical western diet high in calories and low in micronutrients pushes mitochondria too far into anabolic mode, turning on the glycolytic and lipogenic switches required for cell growth, proliferation and potentially, chronic inflammatory disease.Griffiths, R., 2018. Mitochondria in Health and Disease: Personalized Nutrition for Healthcare Practitioners. Singing Dragon.
Overeating
- especially refined carbohydrates
- energy within food is effectively captured from sunlight via photosynthesis
- overeating can deliver more ‘sunlight energy’ than mitochondria can deal with – this is literally ‘sunburn’ on a microscopic scale!
- if mitochondria are overwhelmed with excess glucose/food, they have to export much of this extra energy and convert it into fat, and fat (or adipose tissue) in turn produces inflammatory adipokines associated with mitochondrial dysfunction and depressionCao B, Chen Y, Brietzke E, et al. Leptin and adiponectin levels in major depressive disorder: A systematic review and meta-analysis. Journal of Affective Disorders. 2018 Oct;238:101-110. DOI: 10.1016/j.jad.2018.05.008. https://europepmc.org/article/med/29870819 [accessed 2nd November 2020] Woo, C. Y., Jang, J. E., Lee, S. E., Koh, E. H., & Lee, K. U. (2019). Mitochondrial Dysfunction in Adipocytes as a Primary Cause of Adipose Tissue Inflammation. Diabetes & metabolism journal, 43(3), 247–256. https://doi.org/10.4093/dmj.2018.0221, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6581541/ [accessed 2nd November 2020]
Eating too often
- raises insulin and so inhibits mitochondrial quality control through mitophagy, fusion and fission
High blood sugar/glucose
- caused by excess intake of carbohydrates
- high blood sugar can be very damaging to mitochondria as it can overwhelm the mitochondrial electron transport chain, leading to damaging levels of mitochondrial ROS
- Insulin resistance, type 2 diabetes and obesity are all conditions that slow or inhibit mitophagy, meaning that individuals suffering from these conditions will often have dysfunctional, low-energy mitochondria
- samples of muscle from people with insulin resistance have been found to contain 30% less mitochondria than healthy individuals
Poor nutrition
- whole natural foods contain many of the nutrients and cofactors needed by mitochondria to metabolise food for energy
- processed ‘foods’ are usually deficient in key nutrients and antioxidants and will increase mitochondrial stress and dysfunction
Free fatty acids
- insulin resistance and obesity driven by a poor diet raise levels of free fatty acids which are associated with depression and dementiaSripetchwandee, J., Chattipakorn, N., & Chattipakorn, S. C. (2018). Links Between Obesity-Induced Brain Insulin Resistance, Brain Mitochondrial Dysfunction, and Dementia. Frontiers in endocrinology, 9, 496. https://doi.org/10.3389/fendo.2018.00496, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6127253/ [accessed 2nd November 2020] Melo, H. M., Santos, L. E., & Ferreira, S. T. (2019). Diet-Derived Fatty Acids, Brain Inflammation, and Mental Health. Frontiers in neuroscience, 13, 265. https://doi.org/10.3389/fnins.2019.00265, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6448040/ [accessed 2nd November 2020]
Read more about how nutritional imbalances can damage your mental health.
Exercise is a prime example, where small amounts of mitochondrial ROS (Reactive Oxygen Species) lead the body to produce its own antioxidants in response.
This mitochondrial protective response is another type of hormesis called ‘mitohormesis’.Musci, R. V., Hamilton, K. L., & Linden, M. A. (2019). Exercise-Induced Mitohormesis for the Maintenance of Skeletal Muscle and Healthspan Extension. Sports (Basel, Switzerland), 7(7), 170. https://doi.org/10.3390/sports7070170, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6681340/ [accessed 2nd November 2020]
Excess exercise
- exercise is a form of stress
- too much exercise can cause excessive ROS and inflammation, making it very difficult for mitochondria to recover and maintain their integrity
Not enough exercise
- a sedentary lifestyle deprives mitochondria of the low levels of ROS required to trigger mitohormesis, a mitochondria protective process.Musci, R. V., Hamilton, K. L., & Linden, M. A. (2019). Exercise-Induced Mitohormesis for the Maintenance of Skeletal Muscle and Healthspan Extension. Sports (Basel, Switzerland), 7(7), 170. https://doi.org/10.3390/sports7070170, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6681340/ [accessed 2nd November 2020]
- exercise triggers the pathways necessary to build more mitochondria, in a process called mitochondrial biogenesisAllen, J., Romay-Tallon, R., Brymer, K. J., Caruncho, H. J., & Kalynchuk, L. E. (2018). Mitochondria and Mood: Mitochondrial Dysfunction as a Key Player in the Manifestation of Depression. Frontiers in neuroscience, 12, 386. https://doi.org/10.3389/fnins.2018.00386, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5997778/ [accessed 2nd November 2020]
- exercise can initiate protective measures that improve insulin sensitivity and help to restore mitochondrial quality control strategies, such as mitophagy, fission and fusion
Read more about the effects of inappropriate exercise on mental health.
When we sleep, our brain detoxifies largely thanks to the glymphatic system:
- neurotoxic waste in the brain is cleared by the glymphatic system during sleepHablitz, L. M., Plá, V., Giannetto, M., Vinitsky, H. S., Stæger, F. F., Metcalfe, T., Nguyen, R., Benrais, A., & Nedergaard, M. (2020). Circadian control of brain glymphatic and lymphatic fluid flow. Nature communications, 11(1), 4411. https://doi.org/10.1038/s41467-020-18115-2, https://pubmed.ncbi.nlm.nih.gov/32879313/ [accessed 2nd November 2020]
- brain mitochondria can become dysfunctional if neurotoxic waste (such as amyloid beta) accumulate due to insufficient activity of the glymphatic systemParodi-Rullán, R., Sone, J. Y., & Fossati, S. (2019). Endothelial Mitochondrial Dysfunction in Cerebral Amyloid Angiopathy and Alzheimer’s Disease. Journal of Alzheimer’s disease : JAD, 72(4), 1019–1039. https://doi.org/10.3233/JAD-190357, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6917858/ [accessed 2nd November 2020]
- in an animal model of depression, glymphatic system dysfunction was found surrounding the hippocampus and cortexXia, M., Yang, L., Sun, G., Qi, S., & Li, B. (2017). Mechanism of depression as a risk factor in the development of Alzheimer’s disease: the function of AQP4 and the glymphatic system. Psychopharmacology, 234(3), 365–379. https://doi.org/10.1007/s00213-016-4473-9, https://pubmed.ncbi.nlm.nih.gov/27837334/ [accessed 2nd November 2020]
Getting to bed too late and disrupted circadian rhythms
- weakens mitochondria due to loss of mitochondrial quality control (mitophagy)Schmitt, K., Grimm, A., Dallmann, R., Oettinghaus, B., Restelli, L. M., Witzig, M., Ishihara, N., Mihara, K., Ripperger, J. A., Albrecht, U., Frank, S., Brown, S. A., & Eckert, A. (2018). Circadian Control of DRP1 Activity Regulates Mitochondrial Dynamics and Bioenergetics. Cell metabolism, 27(3), 657–666.e5. https://doi.org/10.1016/j.cmet.2018.01.011, https://pubmed.ncbi.nlm.nih.gov/29478834/ [accessed 2nd November 2020]
- blue light from screens is bad for mitochondria as it blocks melatoninBonmati-Carrion, M. A., Arguelles-Prieto, R., Martinez-Madrid, M. J., Reiter, R., Hardeland, R., Rol, M. A., & Madrid, J. A. (2014). Protecting the melatonin rhythm through circadian healthy light exposure. International journal of molecular sciences, 15(12), 23448–23500. https://doi.org/10.3390/ijms151223448, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284776/ [accessed 2nd November 2020]
Inadequate light exposure and lack of sleep can cause hormone imbalances
- which can in turn disrupt mitochondrial functionNollet, M., Hicks, H., McCarthy, A. P., Wu, H., Möller-Levet, C. S., Laing, E. E., Malki, K., Lawless, N., Wafford, K. A., Dijk, D. J., & Winsky-Sommerer, R. (2019). REM sleep’s unique associations with corticosterone regulation, apoptotic pathways, and behavior in chronic stress in mice. Proceedings of the National Academy of Sciences of the United States of America, 116(7), 2733–2742. https://doi.org/10.1073/pnas.1816456116, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6377491/ [accessed 2nd November 2020]
- other hormones such as ghrelin and leptin which control appetite can also be disrupted by lack of sleep, and contribute to overeatingLin, J., Jiang, Y., Wang, G., Meng, M., Zhu, Q., Mei, H., Liu, S., & Jiang, F. (2020). Associations of short sleep duration with appetite-regulating hormones and adipokines: A systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity, 21(11), e13051. https://doi.org/10.1111/obr.13051, https://pubmed.ncbi.nlm.nih.gov/32537891/ [accessed 2nd November 2020], which as we have seen can also damage mitochondria
Inadequate light exposure and lack of sleep can cause neurotransmitter imbalance
- Gaba, serotonin, dopamine all tie in to circadian rhythmsBedrosian, T. A., & Nelson, R. J. (2017). Timing of light exposure affects mood and brain circuits. Translational psychiatry, 7(1), e1017. https://doi.org/10.1038/tp.2016.262, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5299389/ [accessed 2nd November 2020]
Read more about the effects of lack of nature and natural light on mental health.
- mitochondrial dysfunction in gut epithelial cells makes it very difficult for the cells to produce enough ATP to maintain the integrity of cell junctions, which can lead to leaky gutWang, A., Keita, Å. V., Phan, V., McKay, C. M., Schoultz, I., Lee, J., Murphy, M. P., Fernando, M., Ronaghan, N., Balce, D., Yates, R., Dicay, M., Beck, P. L., MacNaughton, W. K., Söderholm, J. D., & McKay, D. M. (2014). Targeting mitochondria-derived reactive oxygen species to reduce epithelial barrier dysfunction and colitis. The American journal of pathology, 184(9), 2516–2527. https://doi.org/10.1016/j.ajpath.2014.05.019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188172/ [accessed 2nd November 2020]
- a leaky gut can lead to inflammasome activation, and plays a role in the microbiota-inflammasome hypothesis of depressionInserra, A., Rogers, G. B., Licinio, J., & Wong, M. L. (2018). The Microbiota-Inflammasome Hypothesis of Major Depression. BioEssays : news and reviews in molecular, cellular and developmental biology, 40(9), e1800027. https://doi.org/10.1002/bies.201800027, https://pubmed.ncbi.nlm.nih.gov/30004130/ [accessed 2nd November 2020]
- in animal models, a cholesterol rich diet was shown to lead to cognitive decline and mitochondrial dysfunction
- high levels of cholesterol were also found in CNS mitochondrial membranes in Alzheimer’s diseaseDesai, R., & Campanella, M. (2019). Exploring mitochondrial cholesterol signalling for therapeutic intervention in neurological conditions. British journal of pharmacology, 176(22), 4284–4292. https://doi.org/10.1111/bph.14697, https://pubmed.ncbi.nlm.nih.gov/31077345/ [accessed 2nd November 2020]
- conversely however, low plasma cholesterol has been noted in depressive patients, particularly those with lack of remission from their symptomsParekh, A., Smeeth, D., Milner, Y., & Thure, S. (2017). The Role of Lipid Biomarkers in Major Depression. Healthcare (Basel, Switzerland), 5(1), 5. https://doi.org/10.3390/healthcare5010005, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5371911/ [accessed 2nd November 2020]
- it is difficult to understand why studies on cholesterol and neurological health are contradictory, but it could be because the brain has its own cholesterol metabolism which is largely independent from the rest of the body
- however, when the blood-brain barrier becomes ‘leaky’, unwanted peripheral cholesterol metabolites may enter the brain – and other required metabolites may become depletedSaeed, A. A., Genové, G., Li, T., Lütjohann, D., Olin, M., Mast, N., Pikuleva, I. A., Crick, P., Wang, Y., Griffiths, W., Betsholtz, C., & Björkhem, I. (2014). Effects of a disrupted blood-brain barrier on cholesterol homeostasis in the brain. The Journal of biological chemistry, 289(34), 23712–23722. https://doi.org/10.1074/jbc.M114.556159, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4156098/ [accessed 2nd November 2020]
- in a similar way to leaky gut, dysfunctional mitochondria in the blood-brain barrier can make it become more leakyDoll, D. N., Hu, H., Sun, J., Lewis, S. E., Simpkins, J. W., & Ren, X. (2015). Mitochondrial crisis in cerebrovascular endothelial cells opens the blood-brain barrier. Stroke, 46(6), 1681–1689. https://doi.org/10.1161/STROKEAHA.115.009099, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4418219/ [accessed 2nd November 2020]
- dysregulated calcium levels can cause destructive excitotoxicity in neuronal cells
- loss of calcium homeostasis is a major cause of dysfunction in the mitochondria
- it can be caused by excitotoxicity (over-activation of glutamate receptors which allow excessive calcium influx), misfolded proteins and the saturated fatty acid palmitate
- mitochondria are sensitive to calcium and respond by making more ATP – excess calcium will overdrive mitochondria leading to their demise
- if calcium homeostasis is not restored, mitochondria may trigger apoptosis and destroy the whole neuron – this is excitotoxicityGriffiths, R., 2018. Mitochondria in Health and Disease: Personalized Nutrition for Healthcare Practitioners. Singing Dragon.
- mitochondria are both a source and target of inflammation
- when in ‘defense mode’ mitochondria shift from producing ATP to supporting pro-inflammatory cytokine productionCulmsee, C., Michels, S., Scheu, S., Arolt, V., Dannlowski, U., & Alferink, J. (2019). Mitochondria, Microglia, and the Immune System-How Are They Linked in Affective Disorders?. Frontiers in psychiatry, 9, 739. https://doi.org/10.3389/fpsyt.2018.00739, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6333629/ [accessed 2nd November 2020]
- if inflammation remains unresolved, mitochondria may become dysfunctional due to mtDNA damage, compromised membranes and low activity of the electron transport chain (needed to produce ATP)Allen, J., Romay-Tallon, R., Brymer, K. J., Caruncho, H. J., & Kalynchuk, L. E. (2018). Mitochondria and Mood: Mitochondrial Dysfunction as a Key Player in the Manifestation of Depression. Frontiers in neuroscience, 12, 386. https://doi.org/10.3389/fnins.2018.00386, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5997778/ [accessed 2nd November 2020]
Read more about how inflammation can cause mental health issues.
Mitochondria, which have evolved from bacteria, are particularly sensitive to damage from toxins such as;
Pharmaceuticals
- statins have been shown to damage mitochondria Broniarek, I., & Jarmuszkiewicz, W. (2016). Statyny a mitochondria [Statins and mitochondria]. Postepy biochemii, 62(2), 77–84. https://pubmed.ncbi.nlm.nih.gov/28132458/ [accessed 2nd November 2020]
- antibiotics – quinolone, aminoglycoside, and β-lactam antibiotics can cause mitochondrial dysfunction
- Mitochondria originally evolved from bacteria and this common ancestry makes them particularly vulnerable to many antibioticsKalghatgi, S., Spina, C. S., Costello, J. C., Liesa, M., Morones-Ramirez, J. R., Slomovic, S., Molina, A., Shirihai, O. S., & Collins, J. J. (2013). Bactericidal antibiotics induce mitochondrial dysfunction and oxidative damage in Mammalian cells. Science translational medicine, 5(192), 192ra85. https://doi.org/10.1126/scitranslmed.3006055, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3760005/ [accessed 2nd November 2020]
Pesticides and herbicides
Pesticides and herbicides are often engineered to damage the mitochondria of pests and plants, so it’s not surprise that our own mitochondria are harmed by these chemicals.Mesnage, R., Defarge, N., Spiroux de Vendômois, J., & Séralini, G. E. (2014). Major pesticides are more toxic to human cells than their declared active principles. BioMed research international, 2014, 179691. https://doi.org/10.1155/2014/179691, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3955666/ [accessed 2nd November 2020]
Moulds
Mycotoxins from mould can lead to excessive levels of oxidative damage and apoptosis in mitochondria.Islam, M. T., Mishra, S. K., Tripathi, S., de Alencar, M., E Sousa, J., Rolim, H., de Medeiros, M., Ferreira, P., Rouf, R., Uddin, S. J., Mubarak, M. S., & Melo-Cavalcante, A. (2018). Mycotoxin-assisted mitochondrial dysfunction and cytotoxicity: Unexploited tools against proliferative disorders. IUBMB life, 70(11), 1084–1092. https://doi.org/10.1002/iub.1932, https://pubmed.ncbi.nlm.nih.gov/30180298/ [accessed 2nd November 2020]
Infections
- VirusesLatif Reshi, Hao-Ven Wang and Jiann-Ruey Hong (August 29th 2018). Modulation of Mitochondria During Viral Infections, Mitochondrial Diseases, Eylem Taskin, Celal Guven and Yusuf Sevgiler, IntechOpen, DOI: 10.5772/intechopen.73036. https://www.intechopen.com/books/mitochondrial-diseases/modulation-of-mitochondria-during-viral-infections [accessed 2nd November 2020]
- Bacteria – mitochondria release ROS to help fight bacterial infections, but are also compromised by many bacteria.Tiku, V., Tan, M. W., & Dikic, I. (2020). Mitochondrial Functions in Infection and Immunity. Trends in cell biology, 30(4), 263–275. https://doi.org/10.1016/j.tcb.2020.01.006, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7126537/ [accessed 2nd November 2020]
Metals
Mercury, cadmium, lead, aluminium and arsenic are all toxic to mitochondria.Blajszczak, C., & Bonini, M. G. (2017). Mitochondria targeting by environmental stressors: Implications for redox cellular signaling. Toxicology, 391, 84–89. https://doi.org/10.1016/j.tox.2017.07.013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5939563/ [accessed 2nd November 2020] Ohlsson, L., Exley, C., Darabi, A., Sandén, E., Siesjö, P., & Eriksson, H. (2013). Aluminium based adjuvants and their effects on mitochondria and lysosomes of phagocytosing cells. Journal of inorganic biochemistry, 128, 229–236. https://doi.org/10.1016/j.jinorgbio.2013.08.003, https://pubmed.ncbi.nlm.nih.gov/23992993/ [accessed 2nd November 2020]
Hydrocarbons
From smoke increase oxidative stress and mitochondrial dysfunction.Pardo M, Qiu X, Zimmermann R, Rudich Y. Particulate Matter Toxicity Is Nrf2 and Mitochondria Dependent: The Roles of Metals and Polycyclic Aromatic Hydrocarbons. Chemical Research in Toxicology. 2020 May;33(5):1110-1120. DOI: 10.1021/acs.chemrestox.0c00007. https://europepmc.org/article/med/32302097 [accessed 2nd November 2020]
Radiation
Radiation has been shown to damage mitochondria. Kam, W. W., & Banati, R. B. (2013). Effects of ionizing radiation on mitochondria. Free radical biology & medicine, 65, 607–619. https://doi.org/10.1016/j.freeradbiomed.2013.07.024 https://pubmed.ncbi.nlm.nih.gov/23892359/ [accessed 29 November 2020] Livingston, K., Schlaak, R. A., Puckett, L. L., & Bergom, C. (2020). The Role of Mitochondrial Dysfunction in Radiation-Induced Heart Disease: From Bench to Bedside. Frontiers in cardiovascular medicine, 7, 20. https://doi.org/10.3389/fcvm.2020.00020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7047199/ [accessed 2nd November 2020]
Endogenous metabolites
in Parkinson’s and Alzheimer’s disease misfolded proteins and neurotransmitter metabolites can be toxic to mitochondria.Wang, X., Becker, K., Levine, N., Zhang, M., Lieberman, A. P., Moore, D. J., & Ma, J. (2019). Pathogenic alpha-synuclein aggregates preferentially bind to mitochondria and affect cellular respiration. Acta neuropathologica communications, 7(1), 41. https://doi.org/10.1186/s40478-019-0696-4, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6419482/ [accessed 2nd November 2020] Chen, J. X., & Yan, S. D. (2007). Amyloid-beta-induced mitochondrial dysfunction. Journal of Alzheimer’s disease : JAD, 12(2), 177–184. https://doi.org/10.3233/jad-2007-12208, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687350/ [accessed 2nd November 2020] Sarafian, T. A., Yacoub, A., Kunz, A., Aranki, B., Serobyan, G., Cohn, W., Whitelegge, J. P., & Watson, J. B. (2019). Enhanced mitochondrial inhibition by 3,4-dihydroxyphenyl-acetaldehyde (DOPAL)-oligomerized α-synuclein. Journal of neuroscience research, 97(12), 1689–1705. https://doi.org/10.1002/jnr.24513, https://pubmed.ncbi.nlm.nih.gov/31420910/ [accessed 2nd November 2020]
Psychological trauma can lead to:
Hormone and neurotransmitter imbalances
- high cortisol, whether acute or chronic, causes an increase of glucose and lipids (to fuel fight or flight) in the bloodPicard, M., McEwen, B. S., Epel, E. S., & Sandi, C. (2018). An energetic view of stress: Focus on mitochondria. Frontiers in neuroendocrinology, 49, 72–85. https://doi.org/10.1016/j.yfrne.2018.01.001, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5964020/ [accessed 2nd November 2020]
- glucose and lipids then need to be processed by the mitochondria, resulting in metabolic stressPicard, M., & McEwen, B. S. (2018). Psychological Stress and Mitochondria: A Conceptual Framework. Psychosomatic medicine, 80(2), 126–140. https://doi.org/10.1097/PSY.0000000000000544, https://pubmed.ncbi.nlm.nih.gov/29389735/ [accessed 2nd November 2020]
- steroid stress hormones such as cortisol and adrenaline have a beneficial effect on mitochondria in small amounts and a detrimental effect when stress is chronic or at a high levelDu, J., McEwen, B., & Manji, H. K. (2009). Glucocorticoid receptors modulate mitochondrial function: A novel mechanism for neuroprotection. Communicative & integrative biology, 2(4), 350–352. https://doi.org/10.4161/cib.2.4.8554, https://pubmed.ncbi.nlm.nih.gov/19721888/ [accessed 2nd November 2020]
- overactivation of the sympathetic nervous system during stress can undermine CNS mitochondria through loss of anti-inflammatory vagus nerve activityLiu, C. H., Yang, M. H., Zhang, G. Z., Wang, X. X., Li, B., Li, M., Woelfer, M., Walter, M., & Wang, L. (2020). Neural networks and the anti-inflammatory effect of transcutaneous auricular vagus nerve stimulation in depression. Journal of neuroinflammation, 17(1), 54. https://doi.org/10.1186/s12974-020-01732-5, https://pubmed.ncbi.nlm.nih.gov/32050990/ [accessed 2nd November 2020] Porges S. W. (2009). The polyvagal theory: new insights into adaptive reactions of the autonomic nervous system. Cleveland Clinic journal of medicine, 76 Suppl 2(Suppl 2), S86–S90. https://doi.org/10.3949/ccjm.76.s2.17, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108032/ [accessed 2nd November 2020] Shytle, R. D., Mori, T., Townsend, K., Vendrame, M., Sun, N., Zeng, J., Ehrhart, J., Silver, A. A., Sanberg, P. R., & Tan, J. (2004). Cholinergic modulation of microglial activation by alpha 7 nicotinic receptors. Journal of neurochemistry, 89(2), 337–343. https://doi.org/10.1046/j.1471-4159.2004.02347.x, https://pubmed.ncbi.nlm.nih.gov/15056277/ [accessed 2nd November 2020]
- insulin resistance
- chronically high glucose levels due to chronically high stress can lead to insulin resistancePicard, M., McEwen, B. S., Epel, E. S., & Sandi, C. (2018). An energetic view of stress: Focus on mitochondria. Frontiers in neuroendocrinology, 49, 72–85. https://doi.org/10.1016/j.yfrne.2018.01.001, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5964020/ [accessed 2nd November 2020]
- low thyroid hormones – T3 and T2
- T3 and T2 support oxidative phosphorylation (the oxidation of nutrients to make ATP)
- T3 supports mitochondrial biogenesis
- low estrogen
- estrogen, acting through estrogen receptors, supports oxidative phosphorylation, mitochondrial biogenesis, fission and fusionKlinge C. M. (2008). Estrogenic control of mitochondrial function and biogenesis. Journal of cellular biochemistry, 105(6), 1342–1351. https://doi.org/10.1002/jcb.21936, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2593138/#!po=11.9048 [accessed 2nd November 2020]
Increased production of ROS
- chronic psychological stress drives the production of ROS in mitochondria, by undermining oxidative phosphorylation (the oxidation of nutrients to produce ATP) in mitochondriaManoli, I., Alesci, S., Blackman, M. R., Su, Y. A., Rennert, O. M., & Chrousos, G. P. (2007). Mitochondria as key components of the stress response. Trends in endocrinology and metabolism: TEM, 18(5), 190–198. https://doi.org/10.1016/j.tem.2007.04.004, https://pubmed.ncbi.nlm.nih.gov/17500006/ [accessed 2nd November 2020]
Mitochondrial DNA (mtDNA) leaking into the bloodstream
- people exposed to psychological stress have been shown to have mtDNA in their bloodWang, X., Sundquist, K., Rastkhani, H., Palmér, K., Memon, A. A., & Sundquist, J. (2017). Association of mitochondrial DNA in peripheral blood with depression, anxiety and stress- and adjustment disorders in primary health care patients. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology, 27(8), 751–758. https://doi.org/10.1016/j.euroneuro.2017.06.001, https://pubmed.ncbi.nlm.nih.gov/28647451/ [accessed 2nd November 2020]
- mtDNA can be detected in blood plasma of depressive patients and suicide attempters
- components of mitochondria, such as mtDNA, are seen as danger signals once outside mitochondria – don’t forget that mitochondria used to be bacteria
- escaped mitochondrial components are known as DAMPs (damage-associated molecular pattern) and trigger an inflammatory immune responseGrazioli, S., & Pugin, J. (2018). Mitochondrial Damage-Associated Molecular Patterns: From Inflammatory Signaling to Human Diseases. Frontiers in immunology, 9, 832. https://doi.org/10.3389/fimmu.2018.00832, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5946030/ [accessed 2nd November 2020]
- ATP inside a cell provides the cell with energy, but once outside a cell, along with its products ADP, AMP and adenosine, it forms part of the purinergic signalling system
- imbalances in the purinergic system are seen in depression and, interestingly, it is thought that caffeine exerts its antidepressant effects by blocking purinergic receptorsBartoli, F., Burnstock, G., Crocamo, C., & Carrà, G. (2020). Purinergic Signaling and Related Biomarkers in Depression. Brain sciences, 10(3), 160. https://doi.org/10.3390/brainsci10030160, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7139781/ [accessed 2nd November 2020]
Read more about the effects of psychological trauma on mental health.
As we age we lose mitochondrial function
- ageing results in increased mtDNA mutations and reduced mitochondrial ATP productionSrivastava S. (2017). The Mitochondrial Basis of Aging and Age-Related Disorders. Genes, 8(12), 398. https://doi.org/10.3390/genes8120398, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5748716/ [accessed 2nd November 2020]
- it is estimated that age-related neuronal reductions in ATP that exceed 20% may lead to neurological disease
- the good news is that exercise can initiate mechanisms to repair mutated mtDNA and stimulate mitochondrial biogenesis
- appropriate exercise is therefore essential throughout life, particularly in our later years, to keep our neurons and synapses energised and free from diseaseSeo, D. Y., Lee, S. R., Kim, N., Ko, K. S., Rhee, B. D., & Han, J. (2016). Age-related changes in skeletal muscle mitochondria: the role of exercise. Integrative medicine research, 5(3), 182–186. https://doi.org/10.1016/j.imr.2016.07.003, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5390452/ [accessed 2nd November 2020]